Health
- Details
- Written by: Editor
Adventist Health Clear Lake was one of 111 California hospitals in 2018 to be awarded with a Smart Care Award for reducing C-sections.
“Our goal is to provide quality care that helps families grow and flourish,” said Colleen Assavapistkul, the hospital’s vice president of patient care. “As a mom myself, I am very proud that we are encouraging women with low risk to avoid unnecessary surgeries.”
Although cesarean, or C-section, births can be lifesaving when medically needed, national reports show that they are performed for other reasons in some hospitals.
The statistics around low-risk cesarean births prompted the federal government to set ambitious goals to reduce these types of procedures as part of the Office of Disease Prevention and Health Promotion’s Healthy People 2020 targets.
“The decline in California’s rate for low-risk, first birth C-sections will lead to healthier babies and mothers,” said California Health and Human Services Secretary Diana Dooley. “Thanks to the hospitals and their staff for their hard work in achieving this measurable progress.”
Adventist Health Clear Lake’s Women’s Care Unit staff is proud of how it collaborates with families, physicians, and the team providing prenatal and childbirth education services at Adventist Health Clear Lake Medical Offices throughout Lake County to avoid unnecessary C-sections.
“Childbirth is a natural process, and we work with mothers to optimize this amazing moment in their lives,” said Dr. Kimberly Fordham, family medicine and obstetric physician at the Adventist Health Clear Lake Medical Office in Middletown. “Sometimes cesareans are necessary for the mom and/or baby’s health, and we certainly intervene when needed, but our Women’s Care Unit staff and providers have many skills and tools to help most women deliver naturally.”
While life-saving in some circumstances, unnecessary C-sections can pose serious risks to mothers – higher rates of hemorrhage, transfusions, infection and blood clots – and babies, who can experience higher rates of infection, respiratory complications and neonatal intensive care unit stays.
Adventist Health Clear Lake’s Women’s Care Unit provides labor and delivery services to nearly 200 women and their infants each year. The unit is staffed by highly-trained doctors, Certified Nurse Midwives, experienced labor and delivery nurses and other professionals focused on providing the specialized care pregnant women and newborns need.
Growing families can learn more about Adventist Health Clear Lake’s family birth services, including childbirth education classes, at www.adventisthealthclearlake.org in the Services section.
- Details
- Written by: Editor
LAKEPORT, Calif. – Sutter Lakeside Hospital celebrated Patient Safety Awareness Week this week, a time to remind hospital staff and leaders that everyone is a patient.
The Institute for Healthcare Improvement developed Patient Safety Awareness Week to dedicate time and a platform to increase awareness about patient safety among health professionals and the public, according to their website.
“The only difference between us and our patients is a matter of circumstance,” said Dan Peterson, Chief Administrative Officer, Sutter Lakeside Hospital. “Patient Safety Awareness Week serves as a reminder that our patients are our neighbors, friends, coworkers and family. It’s our duty to continue putting patient safety at the forefront of care.”
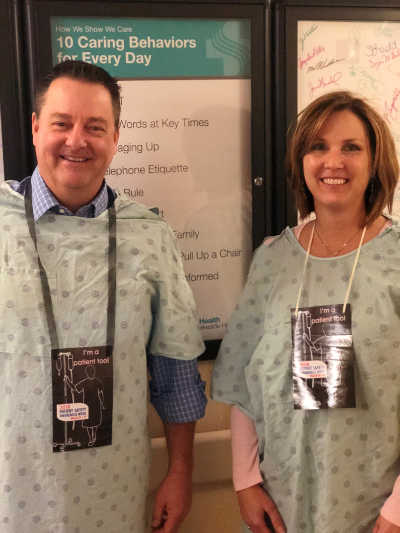
Members of the management team wore hospital gowns and carried “I’m a patient too!” signs throughout the day Thursday as a way to spark discussion about patient safety with staff.
“We recognize the importance of providing safe care, and believe that a culture of safety begins with leadership,” said Peterson. “We encourage staff to speak up when they feel uncomfortable, and challenge the idea that authority exists in a hierarchy. Caring for patients safely is everyone’s responsibility.”
Safety initiatives range from training staff on communicating concerns to using bed alarms to alert nurses when a patient needs help. Metrics such as sepsis mortality rates, hospital-acquired infection rates, pressure ulcer counts and hand washing audits track the quality of care as it relates to patient safety.
“Quality metrics are determined by Sutter Health in accordance with the Joint Commission and federal regulations,” said Peterson. “Sutter Lakeside is graded on those metrics, and we have achieved full performance for over 36 consecutive months.”
Sarah Krevans, president and CEO of Sutter Health, recently recognized Sutter Lakeside as a top hospital in the system for quality and service in 2017 by awarding two presidential dashboard awards. The system award joins a list of recent accolades, such as the Center for Medicare and Medicaid Services’ four star rating of the hospital’s quality metrics.
“We’re incredibly proud of our team’s achievements,” said Peterson. “Ultimately, it means that we’re taking great care of our patients.”
- Details
- Written by: Editor
"A healthy United States is a strong United States. A prepared nation is a safe nation. But persistent underfunding of the country's public health system has left the nation vulnerable," said John Auerbach, president and CEO, of TFAH. "The country needs a long-term commitment to rebuild the nation's public health capabilities – not just to plug some of the more dangerous gaps but to make sure each community will be prepared, responsive and resilient when the unexpected occurs."
Flat federal funding
In Fiscal Year (FY) 2017, the U.S. Centers for Disease Control and Prevention's (CDC) budget was $7.1504 billion ($21.95 per person). Adjusting for inflation, CDC's core budget-not including the Prevention and Public Health Fund-has been essentially flat for the last decade.
Because much of CDC's budget is distributed to states and localities, the impact of budget cuts is experienced directly at the state and local level. Of the roughly 75 percent of CDC funds that go to states and local communities, support ranges from a low of $5.74 per person in Missouri to a high of $114.38 per person in Alaska.
In addition, 12 percent of CDC's budget consists of the Prevention and Public Health Fund, with about $625 million a year of that directed to state and local efforts.
From FY 2013 through FY 2027, the Prevention Fund will receive nearly $12 billion less than the law intended.
Within CDC, the Public Health Emergency Preparedness (PHEP) Cooperative Agreement Program is the only federal program that supports the work of state and local health departments to prepare for and respond to emergencies.
Except for one- time, short-term funding to contain the Ebola and Zika viruses, core emergency preparedness funding has been cut by more than one-third (from $940 million in FY 2002 to $667 million in FY 2017) since the program was established.
State public health funding declining
Spending for public health by states has been declining. Based on a TFAH analysis (adjusted for inflation), 31 states made cuts to their public health budgets from FY 2015-2016 to FY 2016-2017. Only 19 states and Washington, D.C. maintained or increased their budgets, making it hard for states to compensate for reduced federal funding.
According to the report, state public health spending is actually lower in 2016-2017 than it was in 2008-2009, as some of the funding cuts that occurred during the Great Recession have not been fully restored-and federal funding has been essentially flat (almost half of state public health spending comes from federal funds).
Local public health funding decreasing
Since 2008, local health departments (LHDs) have lost 55,590 staff due to layoffs or attrition. In addition, about 25 percent of LHDs reported a lower FY 2016 budget than the previous year, with fewer LHDs reporting an increase in their budget for the current year as compared to the previous.
Recommendations
"Each year, we issue this report to examine the amount of public health funding each state receives and provide an independent analysis of how communities protect the public's health. With life expectancy declining in the U.S. for the second year in a row-something unheard of in recent memory-policymakers must take the public's health seriously and allocate the funds needed to improve well-being and prevent illness and injury," said Auerbach.
The report includes eight key recommendations:
– Increase funding for public health – at the federal, state and local levels.
– Preserve the prevention and public health fund.
– Prepare for public health emergencies and pandemics.
– Establish a standing public health emergency response fund.
– Build a national resilience strategy to combat deaths of despair prevent and reduce chronic disease.
– Support better health and top local priorities in every community.
– Expand the use of evidence-based, high-impact strategies to improve health in every community.
The full analysis is available at www.healthyamericans.org.
Trust for America's Health is a non-profit, non-partisan organization dedicated to saving lives by protecting the health of every community and working to make disease prevention a national priority. www.healthyamericans.org.
- Details
- Written by: Editor

WILLITS, Calif. – Ace Barash, MD has been named Medical Officer of Adventist Health Howard Memorial, or AHHM.
Aside from his new leadership role, Dr. Barash will also continue his role as director of inpatient care, overseeing the care of those hospitalized.
In his new position, Dr. Barash will focus on quality of care, patient experience, medical staff relations and growth at Howard.
“Ace has always championed our mission and unique culture at Howard. He is loved by patients and staff and respected by his colleagues. He cares deeply for this community and we are honored that he’s chosen to continue to share his expertise and skill with Howard in this new leadership position,” shares Jason Wells, Adventist Health Howard Memorial hospital president.
“I believe partnering with physicians in managing through the complexities of the current healthcare landscape is essential. Having Ace share his insights and representing the medical staff at our hospital and clinic leadership meetings will be an asset that will future push us forward to being the exceptional healthcare provider for our community that our region deserves,” Wells explains.
Dr. Barash returned to Howard in 1998 after a hiatus during which he engaged in the private practice of internal medicine.
He had reestablished contact with a well-known local surgeon who was also a good friend and was convinced to return to practicing at Howard.
He has served as a physician in the region for nearly four decades and first cared for patients in the Emergency Room at AHHM in 1983.
After years of private practice, Dr. Barash says it was a breath of fresh air to partner with a hospital, and Howard was the perfect place for him.
Aside from his dedication to his patients, Dr. Barash is also known for his efforts to improve the community as whole. He has been a staunch supporter of improving mental health services in Mendocino County, a cause that is very close to his heart.
“Having seen so many patients in the ER with mental health issues, I felt guilty that I could not do more for my patients. I felt like it was my job to not only address their health issues but also address the underlying mental health issues,” he said.
He is now part of the Measure B Citizens Oversight Committee, which is tasked with, among other duties, reviewing an annual audit of expenditures and providing recommendations for the Board of Supervisors on the implementation of the mental health initiative which passed last year.
“I care deeply about this hospital and this community. Our staff does a great job and I’ve always been proud of the care we provide. I’m excited to help us improve even more so we can continue to give the very best care to our patients,” he explains.
Dr. Barash received his medical degree from University of Kansas School of Medicine and is board-certified in Internal Medicine.
Visit www.howardhospital.org for more information.