Health
- Details
- Written by: Yasmin Anwar
BERKELEY, Calif. – Vision scientists at the University of California, Berkeley, and the University of Toronto have discovered that naturally occurring molecules known as lipid mediators have the potential to halt the progression of glaucoma, the world’s second-leading cause of blindness.
Their findings, published Monday in the online edition of the Journal of Clinical Investigation, mark a major step forward in the pursuit of a cure for glaucoma, a neurodegenerative disease in which fluid buildup in the frontal eye causes irreversible damage to the optic nerve and vision loss.
At present, there is no cure for glaucoma, which is estimated to affect 80 million people worldwide.
“Not only could this discovery lead to drugs to treat glaucoma, but the same mechanism, and options for prevention, may be applicable to other neurodegenerative diseases,” said study senior author Karsten Gronert, professor of optometry and chair of vision science at UC Berkeley.
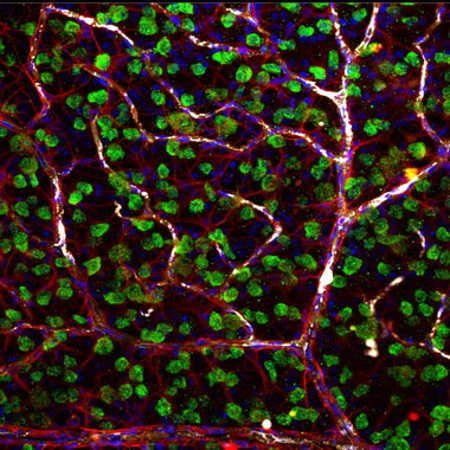
Using rodent models, Gronert and fellow researchers found that inflammation-regulating lipid mediators known as lipoxins, secreted from star-shaped cells known as astrocytes, stopped the degeneration of retinal ganglion cells in rats and mice with glaucoma. Ganglion cells are the neurons of the retina and optic nerve that receive information from photoreceptors.
“We’ve taken something everyone assumed was anti-inflammatory, and found that these same small molecules play a key role in neuroprotection, which is really exciting,” said study co-senior author John Flanagan, dean and professor of optometry. Much of the study was conducted at UC Berkeley.
Specifically, researchers found that astrocytes, which help maintain brain function and form the nerve fiber layer of the retina and optic nerve, release therapeutic biological agents known as lipoxins A4 and B4, but only when the astrocytes are at rest and maintaining nerve function.
“It is commonly assumed that astrocytes activated by injuries release stress signals that kill off ganglion cells in the retina, causing optic nerve damage,” said Flanagan. “However, our research discovered that astrocytes that are triggered by injury actually turn off novel neuroprotective signals that prevent optic nerve damage.”
Researchers discovered secretions of lipoxins A4 and B4 in resting astrocytes in culture in the retina and optic nerve head. To test their potential as a treatment, they administered the lipoxins to rodents eight weeks after the onset of glaucoma-like damage and neurodegeneration.
At 16 weeks, they gauged electrical activity in the rodents’ ganglion cells, among other measures, and found that lipoxin B4 in particular stopped the cells’ degeneration.
“This little-known lipid mediator has shown the potential to reverse cell death,” Gronert said. “We know of no drug that can do this.”
For decades, pharmaceutical companies have searched for neuroprotective drugs to treat glaucoma and other disorders marked by the death of nerve cells such as Alzheimer’s, Parkinson’s and ALS. Glaucoma is by far the most prevalent of these neurodegenerative diseases.
“At the same time, lipoxins have been explored as promising drug targets for treating inflammatory diseases, but nobody has been looking at them as being neuroprotective,” Gronert said.
At present, the treatment option for glaucoma is to lower ocular pressure, but there are no effective treatments for preventing or stopping the neurodegeneration of glaucoma, which is irreversible and eventually leads to blindness, Flanagan said
The study authors are excited at the prospect of further investigations into the therapeutic benefits and mechanisms of lipoxins A4 and B4 and their potential to stop or reverse neural damage. They have jointly filed a patent application for use of lipoxins A4 and B4 to treat glaucoma and neurodegenerative diseases. Their eventual goal is to test the lipoxins as drugs in humans.
"These naturally occurring small lipids have great potential as therapies because they may play a fundamental role in preventing other neurodegenerative diseases. And that's hugely significant, " Flanagan said.
In addition to Flanagan and Gronert, Jeremy Sivak, associate professor of ophthalmology at the University of Toronto, is a senior author on the study. The study’s co-lead authors are Izhar Livne-Bar of the University of Toronto and Jessica Wei and Hsin-Hua Liu of UC Berkeley. Other co-authors are Samih Alqawlaq, Gah-Jone Won and Alessandra Tuccitto of the University of Toronto.
Yasmin Anwar writes for the UC Berkeley News Center.
- Details
- Written by: Editor

CLEARLAKE, Calif. – Adventist Health Clear Lake has collaborated with two local organizations to assist patients who need transportation.
Through a partnership with Lake Transit Authority, or LTA, and a generous gift from Community First Credit Union, Adventist Health Clear Lake now has two vehicles available to shuttle patients to and from important medical appointments.
The partnership with LTA allows the hospital to use a wheelchair-accessible eight-passenger minibus to transport patients who have difficulty getting to and from medical appointments in Lake County.
“Residents who struggle with transportation in Lake County have expressed a need for a service that allows them to not only see their provider, but to accommodate labs and other health screenings following their medical appointments as well,” said Mark Wall, general manager of LTA. “After learning that Adventist Health Clear Lake was fundraising to replace their patient transport vehicle, we approached them about using our available vehicle.”
The bus was put into service by Adventist Health Clear Lake on June 30.
Operated by an Adventist Health Clear Lake driver, the shuttle is already busy taking patients to and from medical appointments around the county.
“It’s crucial that our patients reach their medical appointments as quickly, comfortably and as efficiently as possible,” said Garin Fuhriman, director of outpatient operations at Adventist Health Clear Lake. “Lake Transit has allowed us to better fulfill our shared commitment to those in our community with transportation and health challenges.”
Karl Parker, mobility programs coordinator for LTA, understands the need for non-emergency patient medical transportation in the county.
“LTA dispatchers and I talk regularly with individuals who are unable to take LTA’s fixed-route buses to non-emergency medical appointments because of the distance from their homes to stops, their specific medical issues and other challenges,” Parker said. “Partnerships like these and Lake Links’ Pay Your Pal program are effective, efficient ways to help.”
The partnership with LTA follows Adventist Health Clear Lake’s successful 2016 fundraising campaign for a new vehicle.
The More Than Wheels campaign met its goal thanks in part to a matching challenge grant of $15,000 from Community First Credit Union (formerly Mendo Lake Credit Union).
The challenge grant rallied Adventist Health Clear Lake employees to give over $26,700 in support of the campaign. The result is a 2016 Ford Transit vehicle to replace the aging blue patient bus. The addition of the LTA coach means Adventist Health Clear Lake now has two comfortable, reliable vehicles to transport patients.
“Our vision is to make health care in Lake County as accessible as possible, and collaborating with community partners who share this goal allows us to use our resources to thoughtfully serve our community,” said David Santos, Adventist Health Clear Lake President & CEO. “Through partnerships like this and the work we are doing with the Hope Rising coalition, we are seeing an improvement in quality of life in Lake County.”
Both the new bus purchased by donations from the community and Community First Credit Union and the bus loaned from Lake Transit Authority operate Monday through Friday and travel throughout Lake County.
Patients can request shuttle service when they make their medical appointment at Adventist Health Clear Lake Medical Office locations in Clearlake, Hidden Valley Lake, Kelseyville and Middletown or at the hospital.
- Details
- Written by: Editor
Dr. Fordham is one of 20 physicians to be honored from Adventist Health locations throughout California, Hawaii and Oregon.
Local gynecologist Dr. Paula Dhanda, MD, was honored with the Physician of the Year Alumni Mission Award.
Dr. Fordham has worked with Adventist Health in Lake County for over 13 years. She was nominated by Adventist Health Clear Lake to receive the award because of her dedication to serving local families and her work to support mothers struggling with addiction as the medical director of the Tule House.
The Tule House is a residential addiction treatment program for addicted mothers that provides housing for their children as well.
"I want to give these mothers a peaceful setting where they can realize there is another option," she explains. "Keeping them with their children as they find the healing within themselves helps the entire family."
Aura Palma knows the ripple effect that comes from Dr. Fordham's work with young mothers.
Palma first met Fordham at New Beginnings, an outpatient treatment program in Lake County.
“She really supported me and helped me through some difficult times in my life," Palma said.
Palma beat her addiction, became a nurse and now practices alongside Fordham at the Adventist Health Clear Lake Medical Office -- Middletown as a family nurse practitioner.
Palma and Fordham are creating the Tule House Program together with Redwood Community Services.
"Dr. Fordham is an optimist and a humble person, and she is tenacious," Palma said. "She has tirelessly dedicated herself to this vision because she sees on the front lines what addiction does to mothers and their children, and she believes in their potential like she believed in mine."
Dr. Paula Dhanda, MD, was also honored by Adventist Health with its system-wide Physician of the Year Alumni Mission Award in recognition of her local and worldwide service to women’s health. Through her organization Worldwide Healing Hands, Dr. Dhanda has provided medical care and education in Nepal, Uganda, Chad and Haiti. Worldwide Healing Hands also provides medical care and screenings to the homeless in Lake County. Dr. Dhanda received the Physician of the Year Award in 2010.
Fordham and Dhanda were honored at the Adventist Health Clinical Summit Awards Dinner held in Sacramento, Calif., on Sept. 11.
- Details
- Written by: Editor
NORTH COAST, Calif. – The events of last two weeks have no doubt changed the North Coast’s communities forever.
As fires get close to containment, the road to rebuilding and recovery is just beginning. And whether one was impacted directly by having to evacuate, losing a loved one or just being stressed from the uncertainty of it all, there are many emotions involved.
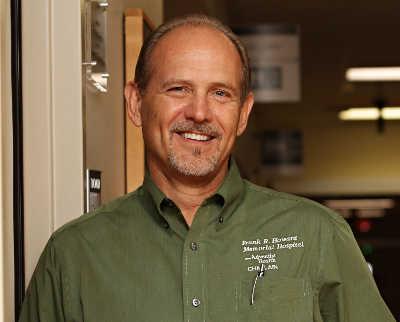
Chaplain Dennis Long, spiritual care director at Frank R. Howard Memorial Hospital in Willits, shared that taking care of one’s emotional and mental health needs are just as important as our physical needs.
“During a disaster, people go into a survival mode and your instincts take over,” he said. “You make it work, you do whatever it takes to protect yourself and your family. But after the adrenaline has worn off, and you start seeing the aftermath, all the stressors are present and the reality of what has happened begins the roller coaster of emotions.”
Long, who offers emotional and spiritual support for patients and their families while in the hospital, says that the feeling of loss one encounters during a death in the family, or getting a cancer diagnosis could also be the same as losing your property, a pet or a job, during a disaster.
Long, who also works with first responders and healthcare workers after a stressful situation, such as the death of a colleague or after a disaster response says it’s important to recognize one’s emotions and hold space for the grief and feeling of loss process; this applies to those directly impacted and those who have family members and friends who have been impacted by the fire.
“Allow yourself to feel those emotions – don’t feel bad about feeling bad,” he said. “Turn to family, a best friend, or a counselor to share your feelings. Take care of yourself first then you can help others by listening, acknowledging that their feelings are normal. The best medicine is to listen and love them. Be respectful of their privacy if they aren’t ready to share their feelings.”
Trained and certified in Critical Incident Stress Management, or CISM, Long has many years of experience facilitating “stress debriefings.”
This week alone, he has done seven debriefings for both hospital staff, first responders and community and his work is just beginning.
“The goal of these events is really to allow people to talk and help them process the emotions. Letting them tell their stories allows them to start processing the disaster and the healing of emotions,” he said.
For those who were not directly impacted, the emotions are still overwhelming.
“Even those who did not have to evacuate, or lost a home will still be going through some stages of grief. And that’s not surprising because we went through this as a community; that comes with being a small town, everyone knows everybody. So we are all affected in some way,” Long said.
For many, just feeling safe again might become a struggle. Going back to doing “normal” things will be hard, but Long said these are normal reactions to an abnormal situation.
“Your world has been rocked. No one ever plans on having to evacuate or losing their home; or just fearing for your family’s lives and your belongings,” he explained.
It might be a challenge but Long said start maintaining a normal schedule, get plenty of rest, and exercise. Do not make any major life changes or decisions, but do make as many daily decisions as, much possible, such as what to eat.
“These small decisions can give you a sense of having control over your life again,” he explained.
A word of caution for well-meaning family members and friends. “The worst thing you can ever say to someone who was directly affected by the disaster is ‘you’re lucky it wasn’t worse,’ or ‘I know how you feel,’” he said. “A traumatized person is not consoled by these statements. Instead, one should just listen and love them. If you feel you need to speak, then say sorry that such a thing has happened to them and that you want to understand and offer help.”
There are also children to think about and Long said most of these tips work as well.
All children need to be reassured that they are safe. The helicopter flying overhead, the sirens of an emergency vehicle can be scary. Your reassurance that they are safe will help their recovery.
“Let the child talk, many times we tend to talk for our children speak for them and not let them really express who they are,” he explained. “Let the child express themselves without interrupting them. It’s like going back to basics, and just sitting down and asking your child, ‘how was your day?’”
Long said older children can cope more effectively with a disaster when they understand what is happening. “Let your child know that it is all right to be upset about what happened and don’t feel obligated to have an explanation for why such a thing happened. Remember, they have a sense of loss as well. Regardless if it’s something small as a toy, to them it’s important. Allow them to express their regrets over “secondary losses” (without accusing them of being selfish or ungrateful).”
Long offered other tips to help cope after a traumatic event such as the recent fires:
- Speak to people or professionals who are willing to listen; “Getting it off your chest” is the most healing medicine. Reach out. People do care.
- Beware of numbing the pain with overuse of drugs or alcohol. Numbing postpones healing.
- Maintain as normal a schedule as possible.
- Give yourself permission to feel rotten, and share your feelings with others.
- Keep a journal; write your way through the sleepless hours.
- Do things that feel good to you.
- Think of three positive things that happened to you each day and think about them before you go to sleep.
- If you are emotionally hurt, scary dreams or flashbacks can occur. Use the tools discussed and they should go away. If not, consult a counselor or chaplain.
- Eat well-balanced and regular meals, even if you don’t feel like it.
SAMHSA also offers a free crisis line for people who have experienced disaster and this can be a good resource for those who need urgent support: 800-985-5990.