Health
- Details
- Written by: Editor
LAKEPORT, Calif. – The Ukiah Valley Rural Health Center-Lakeport is extending hours and adding another day of service.
“I’m excited that we are able to offer extended hours and days for blood draw services,” said Bob MacLafferty, director of laboratory services at Ukiah Valley Medical Center. “We are pleased to offer this convenience to the community, especially since experience has proven that the majority of patients prefer to have their blood drawn early in the morning while fasting.”
UVRH Lakeport lab services will now be available three days per week, Monday, Tuesday and Thursday, from 6 a.m. to 4 p.m.
“When you have your blood drawn at any of our facilities, the testing is performed locally, using local talent, benefitting the local economy, and enabling us to make health care more readily available in our communities,” said MacLafferty.
The UVRHC Lakeport lab is located at 487 S. Main S. in Lakeport, walk-ins are welcome.
For more information please call 707-263-4360.
- Details
- Written by: Editor
Although some advocates want to lower the legal drinking age from 21, research continues to show that the law saves lives.
That's the finding of a new review published in a special supplemental issue to the Journal of Studies on Alcohol and Drugs.
Researchers found that studies done since 2006 – when a new debate over age-21 laws flared up – have continued to demonstrate that the mandates work.
The laws, studies show, are associated with lower rates of drunk-driving crashes among young people. And it seems they also curb other hazards of heavy drinking – including suicide, dating violence and unprotected sex.
“The evidence is clear that there would be consequences if we lowered the legal drinking age,” said lead researcher William DeJong, Ph.D., of Boston University School of Public Health.
The U.S. legal-drinking age has had a winding history. In the early 1970s, 29 states lowered their legal drinking age to 18, 19 or 20.
But after a rise in drunk-driving crashes among young people, many states began to reverse course. A change in federal law eventually pushed all states to adopt a minimum drinking age of 21 by 1988.
But in recent years, the benefits of the age-21 law have been challenged.
In 2006, a nonprofit called Choose Responsibility started campaigning for a change in the federal law.
Two years later, a group of more than 100 U.S. university presidents and chancellors known as the Amethyst Initiative called for a re-evaluation of the legal drinking age – citing a “clandestine” culture of heavy drinking episodes among college students as one reason that the age-21 law is not working.
Those moves grabbed a lot of media attention, and public health experts responded by launching new studies into the impact of the drinking-age law.
Based on DeJong's review, that research supports what earlier work had shown: Since the legal drinking age was set at 21, young people have been drinking less and are less likely to get into drunk-driving crashes.
In one study, researchers found that, in 2011, 36 percent of college students said in the past two weeks they'd engaged in heavy episodic drinking (five or more drinks in a sitting, sometimes called “binge” drinking).
That compared with 43 percent of students in 1988, the first year that all U.S. states had an age-21 law. There was an even bigger decline among high school seniors – from 35 percent to 22 percent.
Of course, many young people break the law and drink anyway. But, DeJong said, the evidence shows that the law is working despite that.
That may be, in part, because minors do not want to be caught drinking, and therefore take fewer risks – like getting behind the wheel.
Plus, DeJong said, “there are many young people who do wait until they're 21 to drink.”
DeJong said that education can help discourage underage drinking. Often, youths buy into the myth, for instance, that all college students engage in heavy drinking episodes. So giving them a more realistic picture of the true “drinking norms” can be effective, DeJong explained.
And, he said, tougher enforcement of the age-21 law, rather than a repeal, is what's needed. “Just because a law is commonly disobeyed doesn't mean we should eliminate it,” DeJong noted.
Clinical trials have found that when college towns put more effort into enforcing the law—and advertise that fact to students – student drinking declines.
“Some people assume that students are so hell-bent on drinking, nothing can stop them,” DeJong said. “But it really is the case that enforcement works.”
- Details
- Written by: Robert Sanders
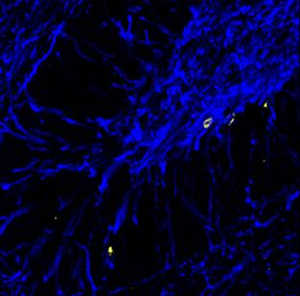
University of California, Berkeley, researchers have shown that chronic stress generates long-term changes in the brain that may explain why people suffering chronic stress are prone to mental problems such as anxiety and mood disorders later in life.
Their findings could lead to new therapies to reduce the risk of developing mental illness after stressful events.
Doctors know that people with stress-related illnesses, such as post-traumatic stress disorder (PTSD), have abnormalities in the brain, including differences in the amount of gray matter versus white matter.
Gray matter consists mostly of cells – neurons, which store and process information, and support cells called glia – while white matter is comprised of axons, which create a network of fibers that interconnect neurons.
White matter gets its name from the white, fatty myelin sheath that surrounds the axons and speeds the flow of electrical signals from cell to cell.
How chronic stress creates these long-lasting changes in brain structure is a mystery that researchers are only now beginning to unravel.
In a series of experiments, Daniela Kaufer, UC Berkeley associate professor of integrative biology, and her colleagues, including graduate students Sundari Chetty and Aaron Freidman, discovered that chronic stress generates more myelin-producing cells and fewer neurons than normal.
This results in an excess of myelin – and thus, white matter – in some areas of the brain, which disrupts the delicate balance and timing of communication within the brain.
“We studied only one part of the brain, the hippocampus, but our findings could provide insight into how white matter is changing in conditions such as schizophrenia, autism, depression, suicide, ADHD and PTSD,” she said.
The hippocampus regulates memory and emotions, and plays a role in various emotional disorders.
Kaufer and her colleagues published their findings in the Feb. 11 issue of the journal Molecular Psychiatry.
Does stress affect brain connectivity?
Kaufer's findings suggest a mechanism that may explain some changes in brain connectivity in people with PTSD, for example.
One can imagine, she said, that PTSD patients could develop a stronger connectivity between the hippocampus and the amygdala – the seat of the brain's fight or flight response – and lower than normal connectivity between the hippocampus and prefrontal cortex, which moderates our responses.
“You can imagine that if your amygdala and hippocampus are better connected, that could mean that your fear responses are much quicker, which is something you see in stress survivors,” she said. “On the other hand, if your connections are not so good to the prefrontal cortex, your ability to shut down responses is impaired. So, when you are in a stressful situation, the inhibitory pathways from the prefrontal cortex telling you not to get stressed don't work as well as the amygdala shouting to the hippocampus, 'This is terrible!' You have a much bigger response than you should.”
She is involved in a study to test this hypothesis in PTSD patients, and continues to study brain changes in rodents subjected to chronic stress or to adverse environments in early life.
Stress tweaks stem cells
Kaufer’s lab, which conducts research on the molecular and cellular effects of acute and chronic stress, focused in this study on neural stem cells in the hippocampus of the brains of adult rats.
These stem cells were previously thought to mature only into neurons or a type of glial cell called an astrocyte.
The researchers found, however, that chronic stress also made stem cells in the hippocampus mature into another type of glial cell called an oligodendrocyte, which produces the myelin that sheaths nerve cells.
The finding, which they demonstrated in rats and cultured rat brain cells, suggests a key role for oligodendrocytes in long-term and perhaps permanent changes in the brain that could set the stage for later mental problems.
Oligodendrocytes also help form synapses – sites where one cell talks to another – and help control the growth pathway of axons, which make those synapse connections.
The fact that chronic stress also decreases the number of stem cells that mature into neurons could provide an explanation for how chronic stress also affects learning and memory, she said.
Kaufer is now conducting experiments to determine how stress in infancy affects the brain's white matter, and whether chronic early-life stress decreases resilience later in life.
She also is looking at the effects of therapies, ranging from exercise to antidepressant drugs, that reduce the impact of stress and stress hormones.
Kaufer's coauthors include Chetty, formerly from UC Berkeley's Helen Wills Neuroscience Institute and now at Harvard University; Friedman and K. Taravosh-Lahn at UC Berkeley's Department of Integrative Biology; additional colleagues from UC Berkeley and others from Stanford University and UC Davis.
Robert Sanders writes for the UC Berkeley News Center.
- Details
- Written by: Editor

LAKE COUNTY, Calif. – On Tuesday, Jan. 14, the Lake County Board of Supervisors provided a forum to launch the countywide Move More 20+14 Challenge.
Move More 20+14 proposes 20 minutes of physical activity daily for the next 14 weeks, as a way to step into 2014 with a resolve to get more physical activity over the course of this year.
Twenty minutes of activity daily comes very close to meeting the 150-minute-per week of physical activity recommended by the nation’s Centers for Disease Control and promoted by numerous other health professionals and organizations.
Physical activity has numerous health benefits, is fun, builds community spirit and is a great way for everyone to combine their energy in lifting up our county’s poor health statistics.
Visit www.movemore2014.org to participate in the challenge, as an individual or as a group.
Since project launch over 675 people (as individuals or as a part of a group) have signed up online.
Several youth are taking photos and posting on the Move More 20+14 Facebook Page ( https://www.facebook.com/groups/movemore2014/ ) about their activities with Rocky the River Otter, a cute plush toy that’s available for groups filled with kids of all ages to join in the fun as they “Rock with Rocky.”
Folks are walking, bowling, running, jump-roping, rowing, playing team sports, hula-hooping and attending various fitness classes from strength training to aerobics, Pilates and yoga.
Everyone is encouraged to do something they enjoy and become part of this exuberant, fun-filled challenge. Taking small steps will lead to BIG rewards of feeling better day by day.
Recent research indicates that sitting too much is becoming the new smoking. Even folks that get regular exercise increase risk for heart disease and diabetes by sitting too much.
Sitting for extended periods of time causes your body to shut down at the metabolic level. When muscles, especially certain leg muscles are immobile, circulation slows. You use less of your blood sugar and burn less fat, which increases risk of heart disease and diabetes.
A 2013 study of nearly 30,000 women found that those who sat nine or more hours a day were more likely to be depressed than those who sat fewer than six hours because prolonged sitting reduces circulation causing fewer feel-good hormones to reach the brain.
In a 12-year study of more than 17,000 Canadians, researchers found that the more time people spent sitting, the earlier they died – regardless of age, body weight, or how much they exercised. Stuart McGill, PhD, director of the Spine Biomechanics Lab at the University of Waterloo says that interrupting sedentary time as often as possible and making frequent posture changes, even taking breaks as short as one minute can improve health.
It’s time to literally stand for health and join the 20+14 MOVEment.
Thanks to each individual who has signed up, to those signing up from sport teams, fitness classes and activity clubs, and to all those organizations that are supporting their employees in forming walking groups, participating in “walking meetings” instead of sitting meetings only, and encouraging taking a hourly break from sitting, as well as promoting other wellness activities.
Thank you to those who are taking on the role of Move More leaders in their group and within organizations.
Move More 20+14 is an activity of “Climb to the Peak of Health”, a countywide collaborative project funded by a Community Transformation Grant awarded to St. Helena Hospital Clear Lake by the Centers for Disease Control.
The goal of the overall grant project is to reduce chronic disease. Schools, businesses, county and community-based organizations and health care are joining together to lift the health status of the community. Your participation is welcomed in this first-time opportunity to find fun ways to increase activity and better our personal and community health.