Health
On the 48th anniversary of the signing of Medicare and Medicaid into law, new information released today by the Department of Health and Human Services (HHS) shows a strong Medicare program.
In California, people with Medicare have saved $573,726,255 on prescription drugs as a result of the Affordable Care Act.
Nationally, these savings average $1,061 per beneficiary in drug costs while a beneficiary is in “donut hole” coverage gap that the law closes over time.
Since the law was enacted, over 6.6 million people with Medicare nationally have saved over $7 billion on drugs.
In addition, 1,375,765 people with traditional Medicare in California took advantage of at least one free preventive service in the first six months of 2013.
This news comes on the heels of historically low levels of growth in Medicare spending. From 2010 to 2012, Medicare spending per beneficiary grew at 1.7 percent annually, more slowly than the average rate of growth in the Consumer Price Index, and substantially more slowly than the per capita rate of growth in the economy.
“Medicare is much stronger as a result of the health care law,” said HHS Secretary Kathleen Sebelius. “Spending has slowed to historic levels, as seniors are enjoying enhanced benefits and greater savings on drugs.”
Savings on prescription drugs
Because of the Affordable Care Act, out-of-pocket savings on medications for people with Medicare continue to grow.
In California, people with Medicare have saved $573,726,255 on prescription drugs in the Medicare Part D donut hole since the law was enacted. Nationally, over 6.6 million people with Medicare have saved over $7 billion, for an average of $1,061.
People with Medicare in the donut hole now receive discounts and some coverage when they purchase prescription drugs at a pharmacy or order them through the mail, until they reach the catastrophic coverage phase.
The Affordable Care Act gave those who reached the donut hole in 2010 a one-time $250 check, then began phasing in discounts and coverage for brand-name and generic prescription drugs beginning in 2011. The law will provide additional savings each year until the coverage gap is closed in 2020.
For more information on how the Affordable Care Act closes the donut hole, please visit: http://www.medicare.gov/part-d/costs/coverage-gap/part-d-coverage-gap.html .
Preventive services
By making certain preventive services available with no cost-sharing obligations, the Affordable Care Act is helping Americans take charge of their own health. Americans can now better afford to work with health care professionals to prevent disease, detect problems early when treatment works best, and monitor health conditions.
In Medicare, the Affordable Care Act eliminated coinsurance and the Part B deductible for recommended preventive services, including many cancer screenings and other important benefits.
For example, before the law’s passage, a person with Medicare could pay as much as $160 in cost-sharing for some colorectal cancer screenings. Today, that screening is free.
In California, 1,375,765 people with traditional Medicare took advantage of at least one free preventive service in the first six months of 2013. Nationally 16.5 million people with Medicare have taken advantage of at least one free preventive service in the first six months of 2013.
- Details
- Written by: Editor
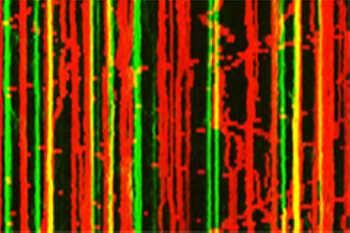
Brain cells talk to each other in a variety of tones. Sometimes they speak loudly but other times struggle to be heard.
For many years scientists have asked why and how brain cells change tones so frequently. On July 25 National Institutes of Health researchers showed that brief bursts of chemical energy coming from rapidly moving power plants, called mitochondria, may tune brain cell communication.
“We are very excited about the findings,” said Zu-Hang Sheng, Ph.D., a senior principal investigator and the chief of the Synaptic Functions Section at the NIH’s National Institute of Neurological Disorders and Stroke (NINDS). “We may have answered a long-standing, fundamental question about how brain cells communicate with each other in a variety of voice tones.”
The network of nerve cells throughout the body typically controls thoughts, movements and senses by sending thousands of neurotransmitters, or brain chemicals, at communication points made between the cells called synapses.
Neurotransmitters are sent from tiny protrusions found on nerve cells, called presynaptic boutons. Boutons are aligned, like beads on a string, on long, thin structures called axons. They help control the strength of the signals sent by regulating the amount and manner that nerve cells release transmitters.
Mitochondria are known as the cell’s power plant because they use oxygen to convert many of the chemicals cells use as food into adenosine triphosphate (ATP), the main energy that powers cells. This energy is essential for nerve cell survival and communication.
Previous studies showed that mitochondria can rapidly move along axons, dancing from one bouton to another.
In this study, published in Cell Reports, Dr. Sheng and his colleagues show that these moving power plants may control the strength of the signals sent from boutons.
“This is the first demonstration that links the movement of mitochondria along axons to a wide variety of nerve cell signals sent during synaptic transmission,” said Dr. Sheng.
The researchers used advanced microscopic techniques to watch mitochondria move among boutons while they released neurotransmitters. They found that boutons sent consistent signals when mitochondria were nearby.
“It’s as if the presence of mitochondria causes a bouton to talk in a monotone voice,” said Tao Sun, Ph.D., a researcher in Dr. Sheng’s laboratory and the first author of the study.
Surprisingly, when the mitochondria were missing or moving away from boutons, the signal strength fluctuated. The results suggested that the presence of stationary power plants at synapses controls the stability of the nerve signal strength.
To test this idea further, the researchers manipulated mitochondrial movement in axons by changing levels of syntaphilin, a protein that helps anchor mitochondria to the nerve cell’s skeleton found inside axons.
Removal of syntaphilin resulted in faster moving mitochondria and electrical recordings from these neurons showed that the signals they sent fluctuated greatly.
Conversely, elevating syntaphilin levels in nerve cells arrested mitochondrial movement and resulted in boutons that spoke in monotones by sending signals with the same strength.
“It’s known that about one third of all mitochondria in axons move. Our results show that brain cell communication is tightly controlled by highly dynamic events occurring at numerous tiny cell-to-cell connection points,” said Dr. Sheng.
In separate experiments the researchers watched ATP energy levels in these tiny boutons as they sent nerve messages.
“The levels fluctuated more in boutons that did not have mitochondria nearby,” said Dr. Sun.
The researchers also found that blocking ATP production in mitochondria with the drug oligomycin reduced the size of the signals boutons sent even if a mitochondrial power plant was nearby.
“Our results suggest that local ATP production by nearby mitochondria is critical for consistent neurotransmitter release,” said Dr. Sheng. “It appears that variability in synaptic transmission is controlled by rapidly moving mitochondria which provide brief bursts of energy to the boutons they pass through.”
Problems with mitochondrial energy production and movement throughout nerve cells have been implicated in Alzheimer’s disease, Parkinson’s disease, amyotrophic lateral sclerosis, and other major neurodegenerative disorders. Dr. Sheng thinks these results will ultimately help scientists understand how these problems can lead to disorders in brain cell communication.
“Our findings reveal the cellular mechanisms that tune brain communication by regulating mitochondrial mobility, thus advancing our understanding of human neurological disorders,” said Dr. Sheng.
- Details
- Written by: Editor
LAKEPORT, Calif. – Sutter Lakeside Hospital’s clinical laboratory has earned The Joint Commission’s Gold Seal of Approval for accreditation by demonstrating compliance with The Joint Commission’s national standards for health care quality and safety in laboratories.
The accreditation award recognizes Sutter Lakeside Hospital’s dedication to continuous compliance with The Joint Commission’s state-of-the-art standards.
Sutter Lakeside’s Clinical Laboratory underwent a rigorous unannounced on-site survey in March.
A team of Joint Commission expert surveyors evaluated Sutter Lakeside Hospital for compliance with standards of care that directly affect the quality and safety of diagnostic services and patient care.
"In achieving Joint Commission accreditation, Sutter Lakeside Hospital’s Clinical Laboratory has demonstrated its commitment to the highest level of care for its patients," said Jennifer Rhamy, M.B.A., M.A., M.T. (ASCP) SBB, HP, executive director, Laboratory Accreditation Program, The Joint Commission. “Accreditation is a voluntary process and I commend Sutter Lakeside Hospital for successfully undertaking this challenge to elevate its standard of care and instill confidence in the community it serves.”
"Achieving Joint Commission accreditation is another demonstration of our commitment to providing the highest levels of quality and safety at Sutter Lakeside,” said Siri Nelson, Sutter Lakeside Hospital chief administrative officer. “Patients are always our first priority. This accreditation validates that we are creating a culture of excellence. Our Clinical Laboratory provides a vital service to Lake County, as it remains open 24 hours a day, seven days a week and provides our clinicians with over 70 percent of our diagnoses. Achieving Joint Commission accreditation is a major step toward maintaining excellence and continually improving the care we provide to our community.”
The Sutter Lakeside Hospital Clinical Lab expanded its services this week by implementing a new rapid in-house test for the detection of Clostridium difficile (C.Diff) glutamate dehydrogenase antigen, toxins A and B to aid in the diagnosis of C. difficile disease.
“C. diff is highly contagious and can compromise a patient’s immune system,” said laboratory manager Hetty Tulloss. “Early detection makes speedy intervention possible. This new test enables us to efficiently identify and treat patients with C. diff and reduces the risk of the disease being spread to other patients and staff.”
The Joint Commission has been evaluating and accrediting laboratory services since 1979. Today, The Joint Commission accredits almost 2,000 organizations providing laboratory services.
Founded in 1951, The Joint Commission seeks to continuously improve health care for the public, in collaboration with other stakeholders, by evaluating health care organizations and inspiring them to excel in providing safe and effective care of the highest quality and value.
The Joint Commission evaluates and accredits more than 20,000 health care organizations and programs in the United States, including more than 10,600 hospitals and home care organizations, and more than 6,600 other health care organizations that provide long term care, behavioral health care, laboratory and ambulatory care services. An independent, not-for-profit organization, The Joint Commission is the nation's oldest and largest standards-setting and accrediting body in health care. Learn more about The Joint Commission at www.jointcommission.org .
To learn more about Sutter Lakeside, please visit www.sutterlakeside.org/ .
- Details
- Written by: Editor
A new test for diagnosing tuberculosis (TB) External Web Site Policy in children detects roughly two-thirds of cases identified by the current culture test, but in a fraction of the time, according to the results of a study in South Africa supported by the National Institutes of Health.
The test, known as Xpert MTB/RIF, also detected five times the number of cases identified by examining specimens under the microscope, a preliminary method for diagnosis that is often performed as an initial test, but which must be verified by the culture test.
Xpert MTB/RIF results from respiratory secretions were ready in 24 hours, on average, compared with an average of more than two weeks for the culture test used in the study, the researchers found.
Previous studies have shown that Xpert MTB/RIF is effective for diagnosing TB in adults and in children with pronounced symptoms of TB who have been admitted to a hospital.
Diagnosing TB in children is more difficult than diagnosing it in adults, because children tend to have much lower levels of the TB bacteria than do adults.
The results of the current study indicated that the ease and speed of diagnosis would be useful for children seen in clinics in resource-limited countries, which often lack the resources for traditional testing that are available in hospitals.
The test also was able to identify children with drug resistant TB. In addition, the researchers found that Xpert can readily determine when treatment for tuberculosis is not appropriate.
Among children who did not in fact have TB, the results of the Xpert test came back negative for TB with 99 percent accuracy.
Xpert MTB/RIF was developed with funding from the NIH’s National Institute of Allergy and Infectious Diseases NIH’s National Institute of Allergy and Infectious Diseases. Testing of Xpert MTB/RIF in children was funded by NICHD.
Preliminary diagnosis of TB is often made by collecting a sample of lung secretions and examining the sample under a microscope to see if it contains the bacteria that cause TB. A sample is also sent to a laboratory so the bacteria can be cultured and identified. It may take as long as six weeks for the culture test to show a positive result.
Because children have lower levels of infectious bacteria than do adults, it is more difficult to detect the bacteria under a microscope and to grow it in a culture. For this reason, accurately diagnosing TB in children has been difficult.
“The availability of this test in primary care settings can help children get appropriate treatment faster,” said Lynne M. Mofenson, M.D., of the Maternal and Pediatric Infectious Disease Branch of the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), the NIH institute that funded the study. “Looking at a specimen under the microscope, often used for initial diagnosis of TB in adults, is very inaccurate in children.”
The Xpert MTB/RIF test also detects TB strains that are resistant to the drug rifampicin, allowing physicians to more accurately prescribe an appropriate treatment, said Carol Worrell, M.D., also of the NICHD’s MPIDB. This is particularly important in areas where drug-resistant TB is common, such as South Africa.
The World Health Organization estimated that in 2011 there were 500,000 TB cases and 64,000 deaths among those younger than 15 years.
The study was led by first author Heather J. Zar, M.D., Ph.D., of the University of Cape Town and Red Cross War Memorial Children’s Hospital, also in Cape Town, South Africa; and Mark P. Nicol, Ph.D, also of the University of Cape Town and the South African National Health Laboratory Service at Groote Schuur Hospital, Cape Town.
The findings appear in The Lancet Global Health.
“There has been a perception amongst health care workers that rapid diagnosis of TB in children wouldn’t be possible in primary care, but this study disproves that view, Dr. Zar said. “Given our results, widespread adoption of rapid testing for TB and drug resistance in children may substantially improve public health without greatly increasing costs.”
Dr. Zar and her colleagues collected almost 1500 samples from nearly 400 children who went to a primary care clinic with symptoms of TB. Collecting the samples – secretions from the lungs, the nasal passages or both – requires special equipment and trained clinical staff.
The researchers compared the results from the Xpert MTB/RIF test, examination of samples under a microscope, and from growing the tuberculosis bacteria in laboratory cultures. Bacterial culture is the most accurate method for diagnosing TB.
Of the 30 TB cases detected by culture, 19 (63 percent) were positive by the Xpert MTB/RIF test on lung or nasal samples, while examining the samples under the microscope turned up only four cases (13 percent). Adding a second test (of a second lung or nasal passage sample) improved the detection rate for both culture and Xpert MTB/RIF
In some cases, researchers started TB treatment for children they suspected had TB based on their symptoms.
Xpert MTB/RIF identified seven children who had clinical symptoms of tuberculosis and responded well to treatment for tuberculosis, but whose tuberculosis had not been detected by the tuberculosis culture test. This might occur when a child is sick with TB, but the bacteria are at especially low levels, or because a sample did not contain enough of the bacteria present in the child’s body to appear when cultured, Dr. Mofenson explained.
The total number of cases detected by culture (30 cases) and by XpertMTB/RIF (26 cases) was similar.
“Because of the global burden of this disease among children, it’s vital to make rapid, accurate diagnostic tests available in primary care settings in order to identify the disease and start treatment before children end up in the hospital,” said Dr. Worrell. “NICHD recognizes the value of supporting research to improve the accuracy of TB diagnosis in children, reduce the number of samples required, and make diagnostic tools widely accessible.”
- Details
- Written by: Editor