Health

UKIAH, Calif. – In mid-July, physical therapist Matt Whitaker, MPT, will open Synergy Physical Therapy Inc., a private practice clinic at 206 Mason St. in Ukiah (adjacent to Yoga Mendocino).
Whitaker has been a physical therapist for more than 15 years, most recently serving as director of physical therapy at Frank R. Howard Memorial Hospital in Willits.
Whitaker is well trained in physical therapy and in business. He had a successful continuing education company for health care professionals and has held clinical and administrative leadership positions over the course of his career.
Whitaker’s approach is hands on and collaborative. He chose the name Synergy because he believes that partnering with patients and physicians achieves optimal results.
“It takes a team approach to provide the best health care and I believe expert treatment combined with patient education and communication with physicians is the best way to accomplish this … When patients come to see me, they should expect measurable improvement in a timely manner,” Whitaker said.
After earning his master’s degree in physical therapy in 1998,Whitaker went on to become certified in vestibular rehabilitation, studying under renowned researcher and author Dr. Susan Herdman of Emory University.
Whitaker also completed a year-long course in manual therapy, studying under Australian-trained physical therapist John Seivert, a nationally recognized speaker whose treatment approach has been the standard of care for many physical therapists. Whitaker has since continued to develop his manual therapy skills through extensive ongoing education.
Whitaker finds that his manual techniques, complimented with appropriate exercise, prove successful to help patients rehabilitate their muscular and nervous systems to return them to normal function.
“I don’t take a ‘one size fits all’ approach. Each patient has individual needs and a unique medical history, so I work with patients to create programs that are tailored to meet their specific goals,” Whitaker said.
Whitaker looks forward to working with many types of patients, from adolescents to elderly adults. He assists patients in recovering from muscular and skeletal injuries or trauma, as well as post-surgical rehabilitation (e.g. after joint replacements). His training with Dr. Herdman focused on balance and fall prevention and vertigo, so he understands how to help older adults (and others) safely get stronger and more stable.
As an athlete himself, he also enjoys sports medicine and helping athletes of all ages recover from injury and return to peak performance. He is working with coaches of local youth sports to help prevent injuries through screenings, education, and strengthening programs.
“In youth sports like basketball and volleyball, we see a number of torn ACLs (a knee ligament). Through sports performance training, I can help young athletes round out their fitness and prevent many of these injuries,” Whitaker said.
Whitaker is also certified as a Level 1 BikeFit Pro through the Seattle-based company, BikeFit. This system offers custom performance fitting for cyclists.
Ensuring a proper fit on a bicycle can be the difference between pedaling efficiently and healthy exercise or compromised performance and potential injury. Having completed multiple Ironman triathlons and numerous marathons, he understands the demands athletes face.
Whitaker said he is looking forward to spending even more time with patients, and anticipates his practice will help meet the pressing physical therapy needs of the community.
Synergy Physical Therapy will be accepting new patients when it opens in mid-July. Learn more by calling 707-462-8080 or visit them online at www.synergypt.net .
- Details
- Written by: Editor
A new study suggests that healthy adults with late bedtimes and chronic sleep restriction may be more susceptible to weight gain due to the increased consumption of calories during late-night hours.
In the largest, most diverse healthy sample studied to date under controlled laboratory conditions, results show that sleep-restricted subjects who spent only four hours in bed from 4 a.m. to 8 a.m. For five consecutive nights gained more weight than control subjects who were in bed for 10 hours each night from 10 p.m. to 8 a.m.
The study found an overall increase in caloric intake during sleep restriction, which was due to an increase in the number of meals consumed during the late-night period of additional wakefulness.
Furthermore, the proportion of calories consumed from fat was higher during late-night hours than at other times of day.
“Although previous epidemiological studies have suggested an association between short sleep duration and weight gain/obesity, we were surprised to observe significant weight gain during an in-laboratory study,” said lead author Andrea Spaeth, a doctoral candidate in the psychology department at the University of Pennsylvania in Philadelphia, Pa.
The study, which appears in the July issue of the journal Sleep, was conducted in the Sleep and Chronobiology Laboratory at the Hospital of the University of Pennsylvania.
The study group comprised 225 healthy, non-obese individuals, ranging in age from 22-50 years. Subjects were randomized to either the sleep restriction or control condition and spent up to 18 consecutive days in the laboratory.
Meals were served at scheduled times, and food was always available in the laboratory kitchen for participants who wanted to eat at other times of day.
Subjects could move around but were not allowed to exercise. They were permitted to watch TV, read, play video games or perform other sedentary activities.
The study also found that during sleep restriction males gained more weight than females, and African Americans gained more weight than Caucasians.
“Among sleep-restricted subjects, there were also significant gender and race differences in weight gain,” said Spaeth. “African Americans, who are at greater risk for obesity and more likely to be habitual short sleepers, may be more susceptible to weight gain in response to sleep restriction. Future studies should focus on identifying the behavioral and physiological mechanisms underlying this increased vulnerability.”
The American Academy of Sleep Medicine reports that weight gain is a risk factor for obstructive sleep apnea (OSA), a common sleep illness that has a severe impact on health and quality of life.
The risk of OSA increases as the degree of additional weight increases, with an extremely high prevalence of OSA in people with morbid obesity.
Anyone who has experienced recent weight gain and has symptoms of OSA, such as loud and frequent snoring, should be evaluated by a board certified sleep medicine physician.
Last week the AASM issued a statement supporting the new policy of the American Medical Association (AMA) recognizing obesity as a disease requiring a range of medical interventions to advance treatment and prevention.
In conjunction with obesity interventions, proper treatment of OSA can dramatically improve overall health and contribute to successful weight management.
- Details
- Written by: Editor
More people are being affected by drug-induced liver injury (DILI) than ever before, according to a new study in Gastroenterology, the official journal of the American Gastroenterological Association.
This type of liver injury results from the use of certain prescription and over-the-counter medications, as well as dietary supplements, and is among the more challenging forms of liver disease due to its difficulty to predict, diagnose and manage.
Investigators conducted a population-based study in Iceland uncovering 19.1 cases of drug-induced liver injury per 100,000 inhabitants, per year.
These results are significantly higher than the last population-based study of this kind, conducted in France from 1997-2000, which reported 13.9 cases per 100,000 inhabitants, per year.
The most commonly implicated drugs were amoxicillin-clavulante (penicillin used to fight bacteria), azathioprine (an immunosuppressive drug used in organ transplantation and autoimmune diseases) and infliximab (also used to treat autoimmune disease).
“Drug-induced liver injury is not a single, uncommon disease of the general population, but rather a series of rare diseases that occur only in persons who take specific medications,” said Einar S. Björnsson, lead study author from the department of internal medicine, section of gastroenterology and hepatology, National University Hospital, Reykjavik, Iceland, and faculty of medicine at the University of Iceland.
“Our study identified which medications put patients most at risk for developing liver diseases. With this information, physicians can better monitor and manage patients who are prescribed potentially liver-injuring drugs,” said Björnsson.
The study also showed that drug-induced liver injury was caused by a single prescription medication in 75 percent of cases, by dietary supplements in 16 percent and by multiple agents in 9 percent.
Further, the incidence was similar in women and men, but increased with age; not surprising since the need for medication also increases with age.
Jaundice and other symptoms highly suggestive of liver injury, such as itching, nausea, abdominal discomfort and lethargy, were present in the majority of patients. Most patients had a favorable outcome after receiving care.
- Details
- Written by: Editor
The very system that is meant to protect the body from invasion may be a traitor. These new findings of a study, led by investigators at the Research Institute of the McGill University Health Centre (RI-MUHC), reveal that infection-fighting white blood cells play a role in activating cancer cells and facilitating their spread to secondary tumors.
This research, published today in the Journal of Clinical Investigation has significant implications for both the diagnosis and treatment of cancer.
“We are the first to identify this entirely new way that cancer spreads,” said senior author Dr. Lorenzo Ferri, MUHC director of the Division of Thoracic Surgery and the Upper Gastrointestinal (GI) Cancer Program. “What's equally exciting is medications already exist that are being used for other non-cancer diseases, which may prevent this mechanism of cancer spread or metastasis.”
According to Dr. Ferri, the next steps are to validate if these medicines will work for the prevention and treatment of cancer metastasis, and then to determine the optimal timing and dosing.
Linking infection, inflammation and metastasis
“Our first clue of this association was from our previous research, which showed that severe infection in cancer patients after surgery results in a higher chance that patients will have the cancer return in the form of cancer metastasis,” said Dr. Ferri, who is also an Associate Member of the Rosalind and Morris Goodman Cancer Research Centre and Associate Professor in the Department of Oncology at McGill University. “This led us to investigate the cellular players in the infection, notably neutrophils, the first and most numerous of the white blood cells that are used by the immune system fight off infections.”
Dr. Ferri and his colleagues from McGill University and the University of Calgary used both cultured cells and mouse models of cancer to show that there is a relationship between infection, a white blood cell response (inflammation) and metastasis.
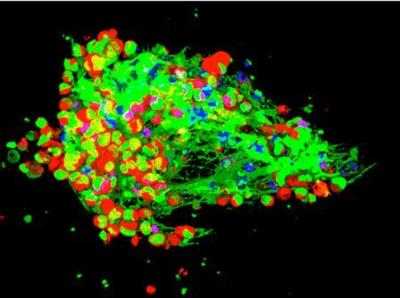
A web-like network called Neutrophils Extracellular Traps (NETs), is produced by white blood cells (neutrophils) in response to an infection and this normally traps and kills invading pathogens, such as bacteria.
“We demonstrated that in the case of infected animals with cancer, the neutrophil web (NETs) also trapped circulating cancer cells,” added Dr. Jonathan Cools-Lartigue, first author of the study, and a PhD student from the LD MacLean Surgical Research Laboratories at McGill University. “Instead of killing the cancer cells, these webs activated the cancer cells and made them more likely to develop secondary tumours, or metastasis.”
No web equals better outcome
The researchers went one step further and showed that breaking down the neutrophil web is achievable by using certain medication.
Furthermore, in mice with cancer, markedly less tumour growth and metastasis occurred after the medication was administered.
This finding was true for a number of different cancer types, suggesting that neutrophil webs may be a common pathway involved in the spreading of many cancers.
“Our study reflects a major change in how we think about cancer progression,” said Dr. Ferri. “And, more importantly, how we can treat it.”
- Details
- Written by: Editor