Health
A 2-year-old child born with HIV infection and treated with antiretroviral drugs beginning in the first days of life no longer has detectable levels of virus using conventional testing despite not taking HIV medication for 10 months, according to findings presented Monday at the Conference on Retroviruses and Opportunistic Infections (CROI) in Atlanta.
This is the first well-documented case of an HIV-infected child who appears to have been functionally cured of HIV infection—that is, without detectable levels of virus and no signs of disease in the absence of antiretroviral therapy.
Further research is needed to understand whether the experience of the child can be replicated in clinical trials involving other HIV-exposed children, according to the investigators.
The case study was presented at the CROI meeting by Deborah Persaud, M.D., associate professor of infectious diseases at the Johns Hopkins Children's Center in Baltimore, and Katherine Luzuriaga, M.D., professor of pediatrics and molecular medicine at the University of Massachusetts Medical School in Worcester. These two pediatric HIV experts led the analysis of the case.
The National Institute of Allergy and Infectious Diseases (NIAID) and the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), both components of the National Institutes of Health, provided funding that supported the work of Drs. Persaud and Luzuriaga and other investigators involved in the analysis of the case.
“Despite the fact that research has given us the tools to prevent mother-to-child transmission of HIV, many infants are unfortunately still born infected. With this case, it appears we may have not only a positive outcome for the particular child, but also a promising lead for additional research toward curing other children,” said NIAID Director Anthony S. Fauci, M.D.
In July 2010, the child was born prematurely in Mississippi at 35 weeks, to an HIV-infected mother who had received neither antiretroviral medication nor prenatal care.
Because of the high risk of exposure to HIV, the infant was started at 30 hours of age on liquid antiretroviral treatment consisting of a combination of three anti-HIV drugs: zidovudine, lamivudine, and nevirapine.
The newborn's HIV infection was confirmed through two blood samples obtained on the second day of life and analyzed through highly sensitive polymerase chain reaction (PCR) testing.
PCR tests conducted on separate occasions that indicate the presence of HIV in an exposed infant are considered to have confirmed the diagnosis of infection.
The baby was discharged from the hospital at 1 week of age and placed on liquid antiretroviral therapy consisting of combination zidovudine, lamivudine and co-formulated lopinavir-ritonavir. This drug combination is a standard regimen for treating HIV-infected infants in the United States.
Additional plasma viral load tests performed on blood from the baby over the first three weeks of life again indicated HIV infection. However, by Day 29, the infant's viral load had fallen to less than 50 copies of HIV per milliliter of blood (copies/mL).
The baby remained on the prescribed antiretroviral treatment regimen until 18 months of age (January 2012), when treatment was discontinued for reasons that are unclear.
However, when the child was again seen by medical professionals in the fall of 2012, blood samples revealed undetectable HIV levels (less than 20 copies/mL) and no HIV-specific antibodies. Using ultrasensitive viral RNA and DNA tests, the researchers found extremely low viral levels.
Today, the child continues to thrive without antiretroviral therapy and has no identifiable levels of HIV in the body using standard assays.
The child is under the medical care of Hannah Gay, M.D., a pediatric HIV specialist at the University of Mississippi Medical Center in Jackson. Researchers will continue to follow the case.
“This case suggests that providing antiretroviral therapy within the very first few days of life to infants infected with HIV through their mothers via pregnancy or delivery may prevent HIV from establishing a reservoir, or hiding place, in their bodies and, therefore, achieve a cure for those children,” said Dr. Persaud.
- Details
- Written by: Editor
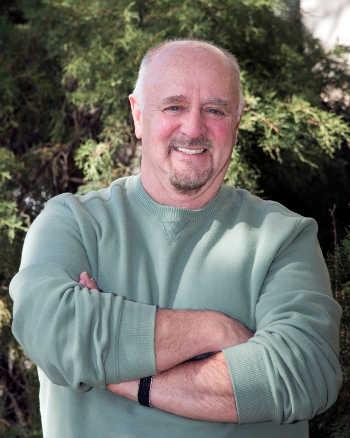
UKIAH, Calif. – In an effort to continually improve patient responsiveness, Mendocino Community Health Clinic (MCHC) recently appointed Wayne Menger to its board of directors.
Menger moved to Ukiah to retire after 12 years as an elementary school teacher in Florida and 15 years with AT&T in California.
Since retiring almost three years ago, Menger has sought opportunities to invest his time and energy in the Ukiah community.
“MCHC is a great match for me. I really like the people, and I truly believe that everyone should have access to health care. At MCHC, everyone is welcome,” he said.
MCHC is a nonprofit health organization that provides primary medical care (including Care for Her), some specialty medical care, dental care, and behavioral health care at three health centers in Ukiah, Willits, and Lakeport.
Because of its designation as a federally qualified health clinic, MCHC brings millions of federal dollars to Lake and Mendocino counties to care for the most vulnerable people in our communities.
Menger was especially impressed with the level of engagement of the current board members. “I’ve volunteered on other non-profit boards, and the thing I liked about the MCHC board meeting is that the people are obviously there to participate, not to pad their resumes. The board members really care,” he said.
Menger hopes to bring his enthusiasm for helping others and his experience from other non-profit boards to MCHC, and believes that not having a health care background will allow him to provide objective feedback from a patient’s perspective.
When he is not working on MCHC business, he also volunteers for the local Humane Society and is on the board of directors at Ukiah Players Theatre.
He and his partner, Victor, both retired in 2010 and enjoy traveling – whether it be to somewhere as close as San Francisco or as far as Europe.
“I think it is so important to really live your life. If you don’t do things now, you may not be able to. We’re living life now,” Menger said.
MCHC CEO Lin Hunter said, “We’re so pleased that Wayne accepted our invitation to join the Board. He is obviously dedicated to giving back to the community and his personality makes him really fun to have at the board meetings.”
- Details
- Written by: Editor
SACRAMENTO – The California Department of Public Health (CDPH) is advising consumers not to eat recreationally harvested mussels, clams or whole scallops from Marin County. Dangerous levels of paralytic shellfish poisoning (PSP) toxins have been detected in mussels from this region; clams and scallops may also pose a health risk.
The naturally occurring PSP toxins can cause illness or death in humans.
This warning is in addition to the annual mussel quarantine that was extended on Oct. 31, 2012, for Del Norte and Humboldt counties. That quarantine remains in effect.
This warning does not apply to commercially sold clams, mussels, scallops or oysters from approved sources. State law permits only state-certified commercial shellfish harvesters or dealers to sell these products. Shellfish sold by certified harvesters and dealers are subject to frequent mandatory testing.
PSP toxins affect the central nervous system, producing a tingling around the mouth and fingertips within a few minutes to a few hours after eating toxic shellfish.
These symptoms are typically followed by loss of balance, lack of muscular coordination, slurred speech and difficulty swallowing. In severe poisonings, complete muscular paralysis and death from asphyxiation can occur. Cooking does not destroy the toxin.
To receive updated information about shellfish poisoning and quarantines, call CDPH’s toll-free “Shellfish Information Line” at 800-553-4133.
For additional information, please visit the CDPH Marine Biotoxins-Mussels frequently asked questions Web page, http://www.cdph.ca.gov/Pages/MusselQuarantineFAQ.aspx .
- Details
- Written by: Editor
Women who reported eating a diet rich in iron were 30 to 40 percent less likely to develop pre-menstrual syndrome (PMS) than women who consumed lower amounts, in a study reported this month by researchers at the University of Massachusetts Amherst School of Public Health and Health Sciences and Harvard.
It is one of the first to evaluate whether dietary mineral intake is associated with PMS development.
Senior author Elizabeth Bertone-Johnson and others at Umass Amherst, with lead author Patricia Chocano-Bedoya and colleagues at Harvard, assessed mineral intake in approximately 3,000 women in a case-control study nested within the prospective Nurses' Health Study II. Participants were free from PMS at baseline.
Women in the study completed three food frequency questionnaires over the 10-year study period. After 10 years, 1,057 women were diagnosed with PMS and 1,968 remained free from PMS.
Adjusting for calcium intake and other factors, the researchers then compared previous mineral intake reported by the women diagnosed with PMS with that of women who had few or no menstrual symptoms.
“We found that women who consumed the most non-heme iron, the form found primarily in plant foods and in supplements, had a 30 to 40 percent lower risk of developing PMS than women who consumed the lowest amount of non-heme iron,” said Bertone-Johnson.
Women in the highest intake group for non-heme iron had a relative risk of PMS of 0.60 compared to women in the lowest intake group.
She added, “We also saw some indication that high intake of zinc was associated with lower risk. In contrast, we were somewhat surprised to find that women consuming the highest amount of potassium had a higher risk of being diagnosed with PMS than women consuming the lowest amount of potassium. In general, results for mineral from food sources and minerals from supplements were similar.”
Overall, “Our findings need to be replicated in other studies. However, women at risk for PMS should make sure they are meeting the RDA for non-heme iron and zinc.
“The level of iron intake at which we saw a lower risk of PMS, roughly greater than 20 mg per day, is higher than the current recommended daily allowance (RDA) for iron for premenopausal women, which is 18 mg per day,” Bertone-Johnson said.
This amount may be obtained in 1 to 1.5 servings per day of iron-fortified cereal or with supplements.
“However, as high iron intake may have adverse health consequence, women should avoid consuming more than the tolerable upper intake level of 45 mg per day unless otherwise recommended by a physician,” she noted.
Iron may be related to PMS because it is involved in producing serotonin, a neurotransmitter that helps to regulate mood, she and colleagues point out.
The unexpected finding of higher PMS risk with high potassium intake, even at levels below current recommendations of 4,700 mg per day, may be related to potassium's role in regulating fluid balance in the body. It may affect PMS symptoms such as swelling in the extremities and bloating by affecting fluid retention.
“More studies of potassium and menstrual symptoms are needed to better understand this,” the researchers said.
“The level of zinc intake at which we saw suggestion of a lower risk of PMS, greater than 15 mg per day, was also higher than current recommendations of 8 mg per day. However, as high zinc intake may also have adverse health consequences, women should avoid consuming more than the tolerable upper intake level of 40 mg per day unless recommended by a physician.”
Intake of other minerals, including magnesium, copper, sodium and manganese were not associated with PMS risk, the authors pointed out.
- Details
- Written by: Editor